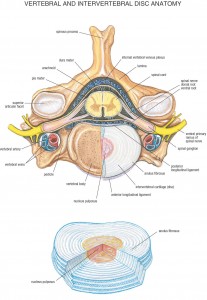
Discogenic pain presents as localized pain at the spine, most often the lumbar spine that worsens with lifting, coughing, sneezing, or straining during a bowel movement. Discogenic pathologies include bulging or herniated intervertebral discs, degeneration of a disc, dehydration of the disc nucleus, or tears in the fibrous capsule (annulus) of the disc. A malformed or degenerated disc can result in the boney vertebrae moving closer together causing peripheral nerve impingement at the neural foramina.
Inversion tables use gravity and your body weight to traction the spine. As the spine stretches, it creates a negative pressure within the intervertebral discs. The negative pressure, in conjunction with osmosis, pulls water into the gelatinous center of the disc called the nucleus pulposus. Stretching and hydration thicken the discs and lengthens the spine. As the discs thicken the separate the vertebra and increase the free space around the nerves as they leave the spine- the result is a healthier and happier you.
What are the contraindications for inversion tables?
Inversion tables take a little coordination and possibly even some assistance. Most inversion tables work by setting the maximum decline angle, locking your ankles into the suspension, then leaning back and slowly tilting backward until your head is below your ankles. This seemingly simple process can be problematic if you have the following issues:
- Retinal detachment
- Stroke
- Recent head injury
- Spinal injury
- Bone weakness
- Lumbar fusions, either surgical or from bone remodeling
- Severe osteoarthritis of the facet joints of the spine
- Tears in the vertebral discs
- Vestibular problems resulting in dizziness and nausea
Geriatric patients or patients with disabilities should not use inversion tables without assistance and clearance from their primary care physician.
When will I feel better?
When patients first begin stretching their spine, it can result in increased discomfort for 1-2 weeks. The reason for this is that the musculature of the spine has contracted to protect and stabilize the injured area. The problem with this is that the increased muscle contraction also creates more pressure on the discs, flattening them out and reducing their ability to rehydrate fully. Increased disc compression with dehydration equals prema ture disc degeneration.
Relief can be immediate but short-lasting. Long-term results will take 4-8 weeks of tractioning five times per week. After the discogenic pain has resolved, a maintenance tractioning program of 3-4 times per week is recommended.
When should I do traction and for how long?
Traction should be performed just before bedtime for 5-10 minutes. Tractioning just before bedtime allows you to lay flat after stretching the discs, so gravity doesn’t recompress the spine before they get a chance to rehydrate.
Stop traction if your pain significantly increases.
Even though your might get slightly worse before getting better, a dramatic worsening in your condition the following traction may indicate that there is a more significant spinal pathology occurring and further diagnosis is required.